We present a case of a 21-year-old female diagnosed with end-stage chronic kidney disease (CKD) of unknown etiology in Guadalajara, Jalisco, Mexico, a city known for its high incidence of CKD at an early age. She had no relevant, known personal medical history or chronic conditions that could have been attributed to the precise etiology of chronic kidney disease.
However, she had a chronic habit of using crystal meth, averaging around 5 grams per day over the last year, which could have exacerbated an underlying cause. Additionally, she was a heavy tobacco user, starting at the age of 15, smoking up to 60 cigarettes a day, with a tobacco index of 18, putting her at moderate risk for chronic obstructive lung disease.
The patient was not living with her family and had a limited social and family support network. She was first admitted in November 2022 after experiencing a chronic episode of diarrhea and abdominal pain. Initially, she sought ambulatory care from general practitioners, who prescribed symptomatic treatment. However, after nearly one and a half months, her pain progressed to become unbearable, accompanied by nausea, vomiting, and fever. She sought medical attention again, and laboratory tests revealed the presence of azotemia, leading to her referral to a secondary-level hospital.
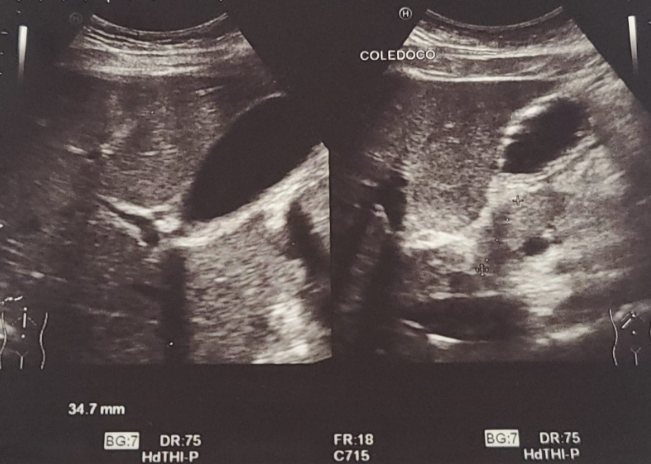
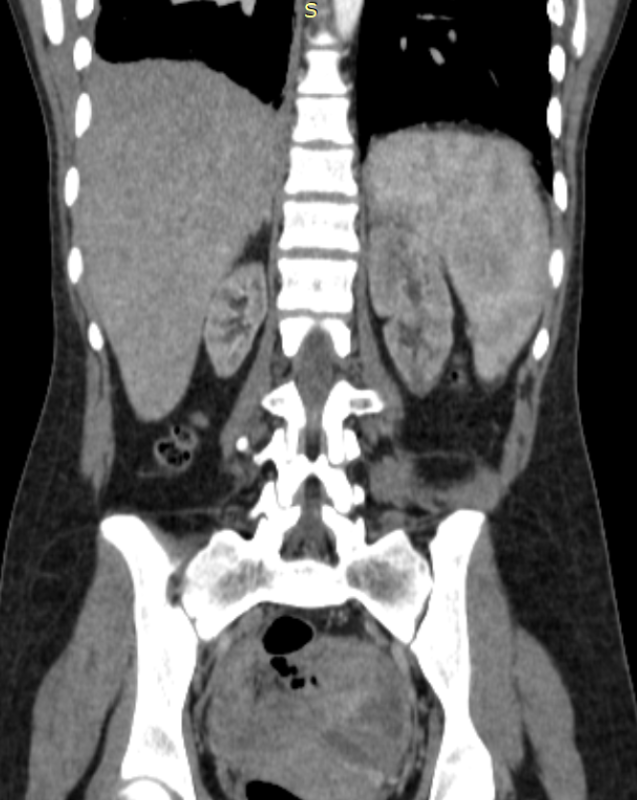
Upon admission, she was evaluated for acute abdominal pain attributed to an acute episode of pancreatitis. An abdominal CT scan was performed, revealing hepatomegaly, bilateral renal hypoplasia, and changes in the cortex/medulla ratio. An abdominal ultrasound showed the presence of an acoustic shadow, suggesting the presence of choledocholithiasis (image 1). Subsequently, a cholangiography resonance scan found that the stones were not obstructing the biliary tract. She received symptomatic treatment to manage gastrointestinal symptoms and was diagnosed with acute kidney injury superimposed on her chronic kidney disease due to an acute episode of biliary pancreatitis.
Despite several days of in-hospital treatment, her azotemia persisted. Laboratory results showed metabolic abnormalities, such as hypocalcemia and azotemia, in conjunction with the imaging findings. She was ultimately diagnosed with end-stage chronic kidney disease after assessment by the nephrology team. She was prescribed predialysis conservative treatment, including bicarbonate, blood pressure control with ACE inhibitors, and diuretics.
The patient was assessed by the nephrology team, and renal replacement therapy was offered to her with hemodialysis. However, the patient declined this treatment and requested voluntary discharge, despite being informed of the risks associated with this decision. Pre-dialysis treatment measures were provided to her to continue her outpatient management and evaluation.
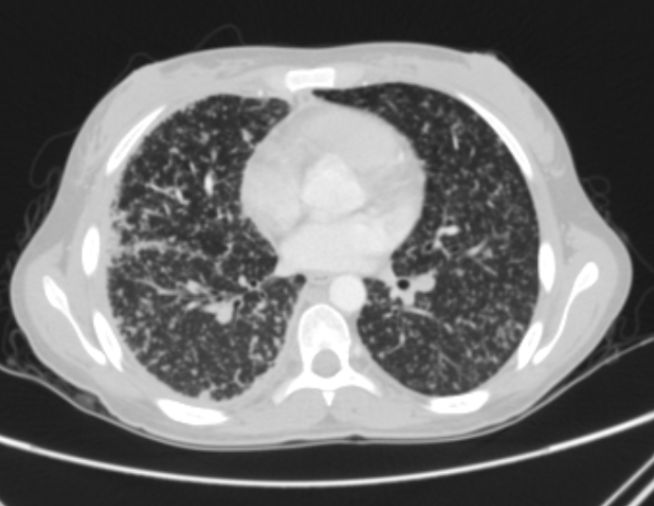
Unfortunately, the patient did not follow the discharge instructions and abandoned her treatment. Two months later, in January 2023, the patient returned to the hospital due to an episode of progressive productive cough with yellowish sputum that persisted throughout the day, accompanied by dyspnea that progressed from exertional to resting dyspnea and orthopnea. She also experienced high-grade intermittent fever and night sweats. X-ray and thoracic and abdominal CT scan images (image 2) suggested an active Mycobacterium tuberculosis lung infection, but not imaging suggesting urinary tract involvement. There was no presence of gallstones in the gallbladder. Even though the three serial Acid-Fast Bacilli (AFB) tests came back negative, she was diagnosed with TB by the infectious disease department.
It came to our attention that, despite not following any of the nephrology team's recommendations and discontinuing all prescribed treatment, she had not received any calcium or other related treatments for mineral bone disorders. She was admitted without symptoms of severely elevated levels of ionized calcium (12.5 mg/dL). Levels of PTH (7.50) and Vitamin D (9.0) (TABLE 1) were requested just before we requested the level of calcitriol; however, the patient escaped from the hospital.
In April 2023, the patient returned to the ED due to persistent signs of active pneumonia, such as dyspnea and a productive cough. She also exhibited symptoms of uremia, including pruritus, nausea, and hyporexia, along with two days of evolving epigastric pain radiating to the left upper quadrants. Her lipase levels were elevated to three times the upper high limit, and her serum calcium levels measured 10.9 with an ionized calcium level of 1.39. She was diagnosed with a new episode of acute pancreatitis. A new POCUS abdominal ultrasound revealed no abnormal findings in the hepatic and biliary tracts. She received analgesics, IV fluids, and pre-dialytic treatment, and her abdominal symptoms improved.
Once again, she was offered renal replacement therapy and TB treatment, but she declined and requested voluntary discharge. As of the time of writing this text, she has not returned to the hospital.