Case one:
A 44-year-old male patient with a pre-hospital scenario of a violin spider (ñandupe) insect bite approximately 15 days ago, presenting cellulitis in the lower limb. He reports delayed consultation and subsequent admission to the Chaco hospital. Twenty-four hours later, he requests voluntary discharge and comes to our hospital, where he is admitted to the Intensive Care Unit for hemodynamic monitoring. The patient is in a fair overall condition, lucid, afebrile, eupneic, with stable hemodynamics requiring vasopressors, a urinary output of 1800 ml/12 hrs, and no presence of edema. Antibiotic therapy with piperacillin + tazobactam and vancomycin is administered, adjusted according to estimated glomerular filtration rate (eGFR). The patient undergoes surgery for debridement of necrotic tissue and fasciotomy in the area affected by the post-spider bite infectious process.
Vital signs:
Blood pressure: 116/60 mmHg Heart rate: 94 bpm Temperature: 36.5°C Oxygen saturation: 99%
Admission diagnoses:
1. Acute Renal Failure
2. Loxosceles spider bite (ñandupe)
3. Septic shock involving skin and soft tissues
4. Necrotizing fasciitis of the right lower limb
5. Immediate postoperative state after debridement and fasciotomy of the right lower limb
6. Cellulitis of the posterior aspect of the right lower limb
7. Type 2 Diabetes Mellitus
Hemodialysis is initiated, and serology for Hepatitis B, Hepatitis C, HIV is requested. Approximately 48 hours after admission to our hospital, daily hemodialysis treatment begins, completing a total of ten sessions.
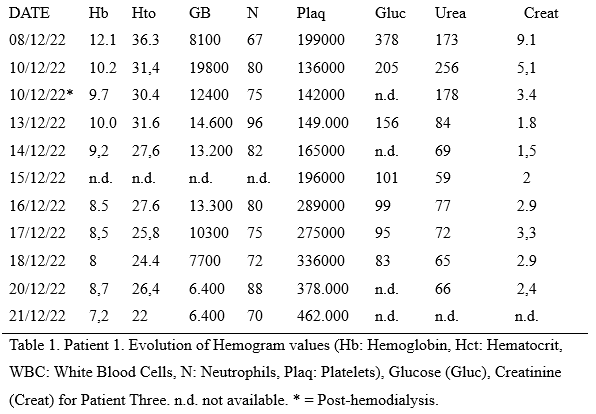
See tabla 1.
Final Diagnoses:
1. Pre-renal Acute Kidney Injury (AKI)
2. Septic shock originating from the skin and soft tissues due to Hemolytic Group A Streptococcus B or pyogenes.
3. Necrotizing fasciitis of the right lower limb.
4. Compartment syndrome of the right lower limb.
5. Postoperative state after debridement and fasciotomy of the right lower limb.
6. Cellulitis of the right lower limb following a spider bite (ñandupe).
7. Type 2 Diabetes Mellitus.
8. Severe anemia.
The patient maintains urinary output through a bladder catheter with physiological values, but with a worsening general condition, leading to a decision to transfer to a more complex hospital where the patient eventually passes away.
Case two:
A 33-year-old male patient with a history of bee stings. Information provided by the patient and accompanying family is credible. They report that approximately 18 days ago, the patient was stung by a wasp. They cannot specify the quantity but describe being completely surrounded, receiving stings on the face, anterior chest, and limbs. Four days ago, he sought medical attention due to general malaise, nausea, vomiting, and respiratory distress, initiating oral treatment. With worsening symptoms, he decided to go to the emergency department at the Regional Hospital of Concepción, where Kussmaul breathing, dry mucous membranes, and a distressed facial expression were observed.
Upon admission, the patient is conscious and cooperative. Stable hemodynamics with a tendency towards tachycardia and hypertension, tachypneic with poor respiratory mechanics. The patient is anuric.
Vital signs:
Blood pressure: 183/110 mmHg Heart rate: 132 bpm.
Oxygen saturation: 95% with supplemental oxygen at 10 liters through a facial mask.
Axillary temperature: 36°C.
Admission to the Adult Intensive Care Unit (AICU):
Admitted on a stretcher, accompanied by nursing staff, with psychomotor agitation, Glasgow Coma Scale 12/15 due to the absence of verbal response, poor respiratory mechanics with oxygen through a facial mask, stable hemodynamics, indwelling urinary catheter with no output.
Sedation and orotracheal intubation are performed for mechanical respiratory assistance (MRA), obtaining central venous access for hydration/medication, and femoral venous access with a double-lumen catheter for hemodialysis.
VITAL SIGNS: HR: 89 BP: 125/67 RR: 16 SPO2: 100% TEMP: 35.5°C
AICU Admission Diagnosis:
1. Acute renal failure.
2. Severe acute respiratory failure requiring MRA.
3. Severe metabolic acidosis.
4. Severe hyperkalemia.
5. Severe dehydration.
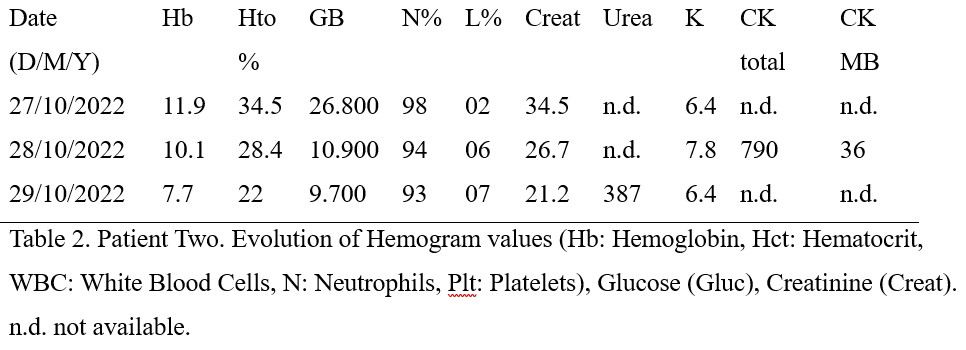
See tabla 2.
An emergency conventional hemodialysis session is initiated with zero net ultrafiltration for two hours, with good tolerance to the treatment.
Final Diagnoses:
1. Spider bite.
2. Pre-renal acute kidney injury.
3. Mixed shock (hypovolemic and septic).
4. Necrotizing fasciitis of the right lower limb.
5. Compartment syndrome.
6. Postoperative state after debridement and fasciotomy of the right lower limb.
7. Cellulitis of the posterior right lower limb.
8. Type 2 Diabetes Mellitus.
9. Severe anemia.
The patient, with a progressively deteriorating general condition, undergoes nine hemodialysis sessions without improvement and eventually passes away on day XX.
Case three:
81-year-old patient with a history of snakebite three days ago, currently experiencing acidotic breathing with O2 support through a facial mask with a reservoir, obstructive-appearing anuria due to a distended bladder. The patient reports having normal urination characteristics before this event, with a history of prostate surgery.
Vital signs:
BP: 184/100 mmHg HR: 97 bpm RR: 31 bpm SPO2: 100%
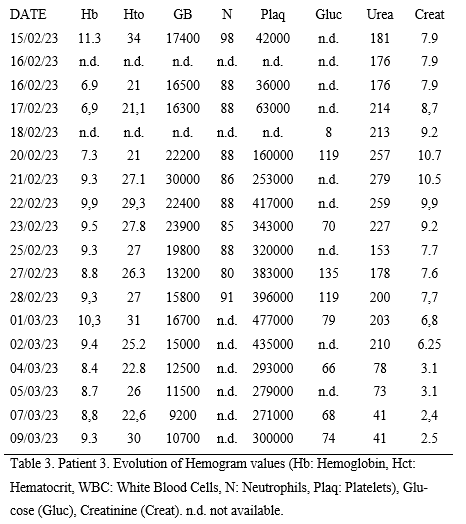
See tabla 3.
Diagnoses:
1. Acute renal failure.
2. Brotropic snakebite.
3. Acute urinary retention of undetermined etiology.
4. Arterial hypertension.