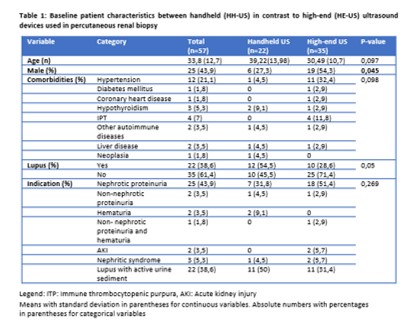
Fifty-seven native kidney biopsies were
performed in the study period, of which 22 (38.9%) were performed with HH-US and 35 (61.4%) with
HS-US.
Of all patients, 56.1% % (n=32) were females and the
mean age was 33,8 ± 12.7 years. The most frequent comorbidity was systemic
lupus erythematosus (38,6%, n=22) followed by arterial hypertension (21,1%, n=12)
and the most common indication for kidney biopsy was nephrotic syndrome (43,9%,
n=25) followed by lupus with active urine sediment (38,6%, n=22) (Table 1).
The biopsy samples were almost always taken from the
left side (96,5% n=55), with a needle gauge of 16 G (91,2% n=52). The
needles were used for a median of 2,2 passes (± 0,5) and collected a median of
15,7 ± 8.1 glomeruli for optical microscopy. Primary glomerular disease (PGD)
was reported in 52,7% (n=30), while secondary glomerular disease was reported
in 44% (n=25) of the biopsies studied. (Table 2).
There were no complications in 82.5% (47 biopsies),
minor complications in 17,5% (10 biopsies) and no major complications of the
procedures. The most frequent minor complications were pain lasting ≥ 12 hours (7%,
n=4), hematoma (7%, n=4) and gross hematuria (3,5%, n=2).
No significant differences in post-biopsy
complications such as pain, hematoma, need for transfusion and intervention,
gross hematuria or infection were observed between HH-US and HE-US. (no
complication in 82,5% HH-US vs 72,7% HS-US, p = 0.39)
The overall adequacy rate of native biopsy was 85,7% (n=
48), with no significant difference among groups (81,8% HH-US vs
88,2% HS-US, p = 0.5).