A 33-year-old male donor, blood group and factor O Rh +, with a history of psoriasis, overweight and alcohol consumption for 13 years, admitted to the emergency room for nausea, dizziness and decreased visual acuity. According to an interview with family members, he had consumed alcoholic beverages the previous day, we did not perform a methanol blood test, the diagnosis of methanol intoxication was clinical, as described below.
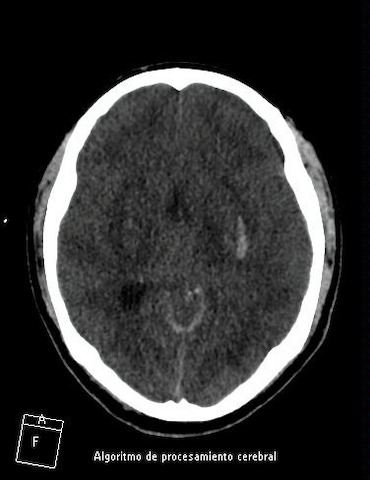
Blood gases showed severe metabolic acidosis with elevated anion gap associated with acute kidney injury (AKI) and poor respiratory pattern requiring mechanical ventilation and the use of vasopressors: noradrenaline and vasopressin. 2 hemodialysis sessions were performed and the acid-base alteration described above persisted (Table 1). Brain tomography showed subarachnoid and intraparenchymal hemorrhage, in addition to cerebral edema (Figure 1). Neurology and intensive medicine corroborate absence of truncal reflexes, with apnea test, atropine test and oculovestibular reflex contributing to brain death. Thus, organ donation procurement was activated, and the family accepts the donation.
A zero renal biopsy was made and the left kidney that was transplanted to our patient had 25 glomeruli, with a total score of 2 points of Ramuzzi scale, 1 for tubular atrophy and 1 for vascular sclerosis.
A deceased donor kidney transplant was carried out on September 3rd, 2022, to a 45-year-old female patient with CKD G5 on dialysis since 2017, peritoneal dialysis modality and uncertain etiology, received immunosuppression: methylprednisolone, antithymocyte globulin, tacrolimus, and mycophenolate sodium. Cold ischemia time of 19 hours. In the immediate postoperative period, there was no consciousness disorders, visual alterations, or elevated gap metabolic acidosis. On postoperative day 2 she presented signs of pulmonary congestion, oliguria and nitrogen retention, so a hemodialysis session was scheduled. Then, she presented favorable evolution, adequate urinary flow, creatinine of 3.52 at discharge, and one month after surgery creatinine of 0.97. She had an episode of urinary tract infection by E. coli BLEE which resolved with antibiotic therapy. One year later, she preserves renal function, with no other complications at the moment. (Table 2).