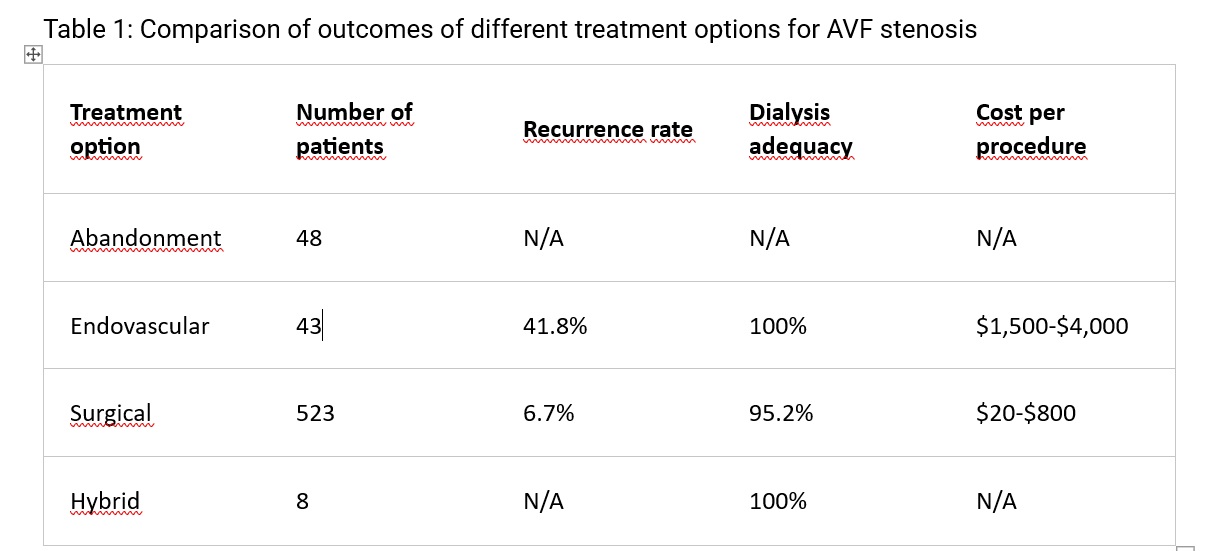
The follow up was at least 12 months.
Of the 671 operated patients, 53 had a recurrence 7.9%, and we had to
re-operate or create a new AVF.
Of the 55 patients treated with angioplasty, 24 had a recurrence 43.6%,
who had the procedure repeated or received surgical treatment.
The recurrence rate
was significantly lower in the surgical group than in the endovascular group (7.9%
vs 43.6%, p<0.001).
The dialysis adequacy
was measured by the Kt/v ratio, which indicates the clearance of urea from the
blood. A Kt/v ratio of more than 1.2 is considered adequate for hemodialysis.
All patients in the endovascular and hybrid groups had adequate dialysis with a
Kt/v ratio of more than 1.2. In the surgical group, 498 patients (95.2%) had
adequate dialysis, while 25 patients (4.8%) needed a temporary catheter because
the repair did not allow an immediate puncture site.
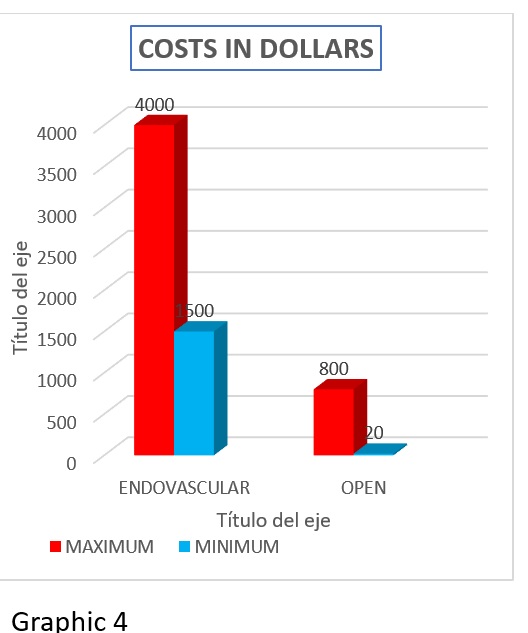
The cost per
procedure was calculated based on the supplies used for each treatment option.
The endovascular treatment required sheaths, wire guides, accessories,
catheters, balloons, insufflators, angiography, stents, and double
antiplatelets. The cost ranged from $1,500 to $4,000 depending on the devices
used. The surgical treatment required sutures and eventual prosthesis. The cost
ranged from $20 to $800 if a prosthesis was used. The hybrid treatment required
both endovascular and surgical supplies, but the exact cost was not available.
The abandonment option did not incur any cost for the treatment of AVF
stenosis, but it required the creation of a new AVF, which was not included in
the analysis.
The
cost-effectiveness analysis showed that the surgical treatment was much more
economical than the endovascular treatment in terms of supplies. The cost of
surgical treatment was between 1.3% and 20% of the cost of endovascular
treatment. For every 100 procedures, the endovascular treatment would cost
between $150,000 and $400,000, while the surgical treatment would cost between
$2,000 and $80,000. Therefore, the endovascular treatment was between 80% and
98% more expensive than the surgical treatment in terms of supplies.
The results at 12
months showed that the surgical treatment had better outcomes than the
endovascular treatment in terms of recurrence rate, dialysis adequacy, and
cost-effectiveness. The hybrid treatment was used for complex cases of aneurysm
and stenosis, but the sample size was too small to draw any conclusions. The
abandonment option was used for cases with low chances of success, but it had
the disadvantage of losing a functional AVF and requiring a new one.